
Celebrity news, beauty, fashion advice, and fascinating features, delivered straight to your inbox!
Thank you for signing up to . You will receive a verification email shortly.
There was a problem. Please refresh the page and try again.
What sounds like the plot of a sci-fi novel is unfolding in a lab in a soaring glass-and-marble I.M. Pei–designed building sprawled on a hillside in Marin County, California. Outside, deer, wild turkeys, coyotes, and the occasional elusive mountain lion roam the 488-acre campus. Inside, Lei Lei, an ovarian biologist recruited from the University of Michigan Medical School, is showing intellectual-property lawyer and legal-tech entrepreneur Nicole Shanahan a magnified image of a mouse ovary. Lei points out the egg cells, which are stained green. “This is a tiny nucleus,” she says, indicating a round speck on the screen. “Very cute!”

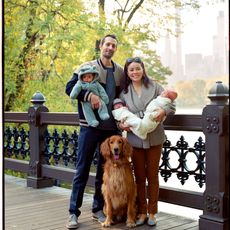
Nicole Shanahan, along with her husband, Sergey Brin, is funding research on the inevitability of menopause.
Lei works at the Buck Institute’s Center for Female Reproductive Longevity and Equality, which was created and funded by Shanahan and her husband, Google cofounder Sergey Brin, in 2018, after Shanahan had trouble getting pregnant. She was 29 when doctors told her that her body possessed such a low number of active ovarian oocytes (immature egg cells) that she wasn’t likely to produce many, if any, eggs and that she appeared to be nearing menopause. She visited several top-notch fertility clinics in the Bay Area, but none were optimistic about her chances of conceiving.
IVF didn’t work for Shanahan; it doesn’t for more than half of women who try it. (The average success rate for an initial IVF embryo transfer is less than 40 percent.) Egg freezing, offered as an employee perk by many top tech companies, including Google, has even slimmer odds.
Shanahan had come face-to-face with what she refers to as “reproductive inequity.” She was irate. Men more than twice her age could father children with little trouble. Why was a woman in her 20s edging into menopause? No one could tell her.
During this time, she was at TV and film producer Norman Lear’s home for a work event. Victor Dzau, president of the National Academy of Medicine, spoke to the group about changing the narrative on aging. As Shanahan listened, she checked her Flo app to see if she was ovulating. Suddenly, it occurred to her: If someone could, in fact, alter this particular aspect of aging, why shouldn’t it be her?
At the wine and cheese reception afterward, Shanahan peppered the scientists in attendance with questions about who was working on halting ovarian aging. She was dismayed to hear that there had been scant research into why women’s ability to bear children spans just a few decades.
“I had always assumed there were good scientific reasons why women can’t reproduce after a certain age,” says Shanahan, now 34, “but they couldn’t cite a paper or a Nobel laureate. They said, ‘I have never thought of that!’”
Someone without Shanahan’s clout, drive, and wallet might simply have taken to social media to vent about the unfairness of it all or started an online petition to draw attention to this latest example of women’s needs being overlooked. But Shanahan took a different route: She committed more than $13 million—some in conjunction with Brin’s foundation (he alone is worth more than $62 billion) and some from her own, the Bia-Echo Foundation—to determine if menopause can be eliminated.
Via the Bia-Echo Foundation, which is investing in reproductive longevity and equality, criminal-justice reform, and healthy-planet initiatives, Shanahan herself is underwriting a $7.4 million global consortium that will provide grants to researchers around the world who are interested in studying female reproductive aging. Another $6 million from the couple went to establishing the aforementioned Center for Female Reproductive Longevity and Equality—the first independent research organization devoted solely to the topic. It is part of the Buck Institute for Research on Aging, and it aims to tackle gaps in knowledge and funding by bringing together scientists who study aging in general with those few who study female reproductive aging and fertility. Their mission, according to a news release, is to address “an inequality which has existed throughout human history: Men can reproduce throughout their life span, but women’s fertility begins to decline in their early 30s.”
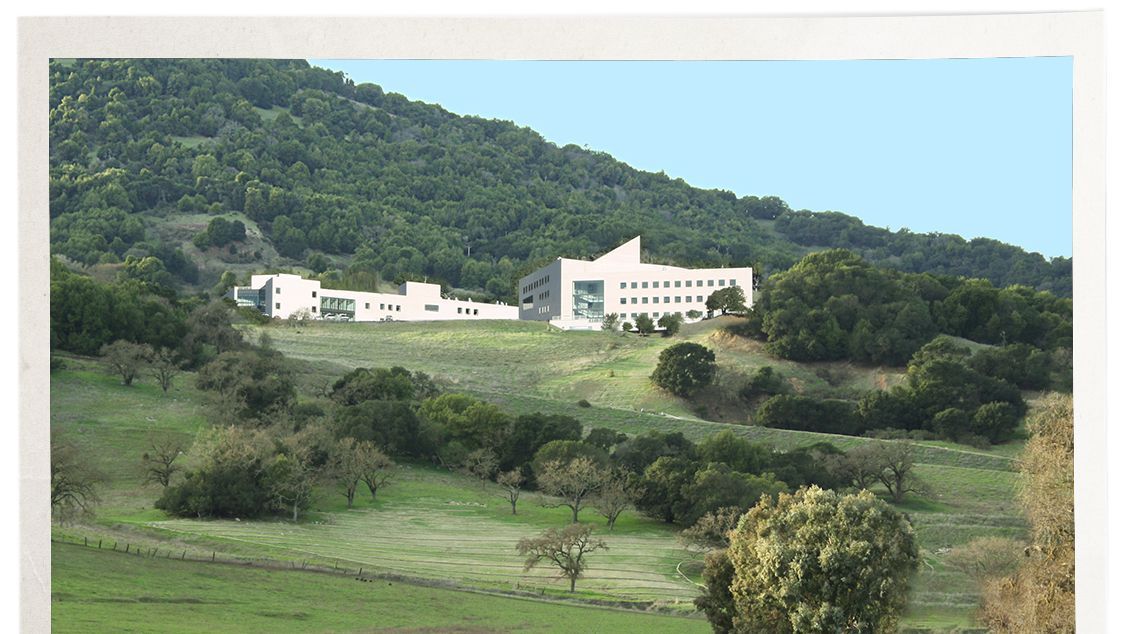
The bucolic I.M. Pei-designed Buck Institute for Research on Aging in Marin County, the site of the Center for Female Reproductive Longevity and Equality.
Shanahan and the scientists are framing this as a feminist cause. (If this were an issue that affected men, Shanahan notes, we’d probably know all the answers already.) Figuring out how to delay menopause and extend the childbearing years could offer women more freedom to pursue a career or find the right partner without getting spooked by the loud and incessant ticking of their biological clocks. It could translate to better health: Once a woman goes through menopause, she may experience a cascade of negative health effects that impact bone, cognitive, cardiovascular, and immune health. If scientists can figure out how to delay reproductive aging, is it possible that women can thrive for longer?
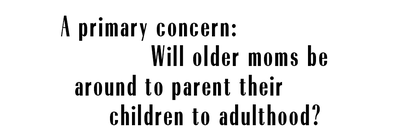
Every month, like clockwork, scientific sleight of hand is taking place deep inside a woman’s body. A single oocyte in a single ovary is anointed the One, transformed into a full-fledged egg, and readied for ovulation. How is that lucky egg selected? Why is a baby girl born with one to two million oocytes, although there’s no way she’ll use more than the tiniest fraction of them? More important, with such a huge surplus of would-be eggs—as women age, they run out of functioning eggs, but eggs don’t disappear—why does women’s fertility have a shelf life?
Plenty of women skip the placebo week of their birth control pills to manipulate their cycles and avoid getting their periods; some women want to sidestep the hassle of bleeding monthly, and others like knowing that their period won’t interrupt a planned vacation or, say, their wedding night. If we can hack menstruation to prevent periods, perhaps we can also do the opposite? This is, quite possibly, the biggest quandary Shanahan’s pursuits—if successful—will have to address: Will women want to keep having menstrual cycles into their 60s and beyond? Shanahan is betting yes—if they understand the benefits.
Menopause is, of course, a biological fact. But Shanahan, who has shown up at the Buck Institute this blue-skied winter day nearly makeup free, with her long brown hair softly curled, doesn’t think it has to be. She is wearing an oatmeal-hued turtleneck, jeans, and suede boots, a counterpoint to the carefully curated business casual of the people she’s meeting with at the Buck. “Doesn’t that sound like the same narrative, that a woman can’t be president or that she can’t be a mother and a CEO at the same time?” Shanahan says. “It’s time to recalibrate our approach. We need to give women greater control over their reproductive future.”
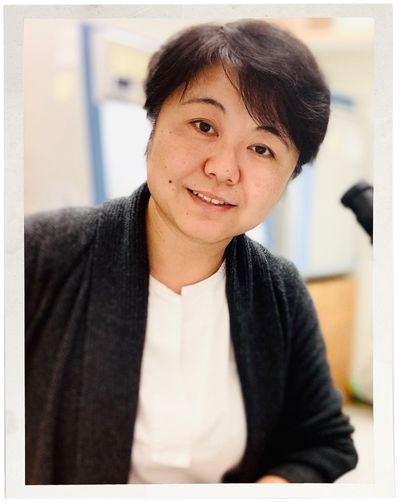
Ovarian biologist Lei Lei delves into the mysteries of reproduction at the Buck Institute.
Most people think of menopause as the time in women’s lives when they stop having periods. That’s true, but it’s only part of the story. Over their reproductive lifetime, women release one egg per month for some 500 months. Then, the walnut-size organs start closing up shop, no longer releasing eggs (though the ovaries still produce some hormones, even after menopause). They’re the first organ in the female body to age in such a profound, literally life-changing way. Studying why these organs quickly deteriorate when they do—and what ignites this change—can provide valuable clues to aging across the board. Jennifer Garrison, an assistant professor at the Buck Institute, thinks of the ovaries as “the canary in the coal mine. Your ovaries start to decline right at the moment when the rest of your tissues are at peak capacity. That’s very odd and potentially very telling in terms of the mechanisms of general aging.”
Starting around age 35, a host of physiological functions, such as maximum breathing capacity and maximum heart rate, begin to decline. Younger hearts can beat faster than older hearts, which is one reason why aerobic workouts get tougher as we age. But these declines happen gradually over many years; in contrast, ovaries decline earlier and more abruptly relative to other organs and, on average, about three decades before a woman dies. (In the U.S., the average age of menopause is 51.)
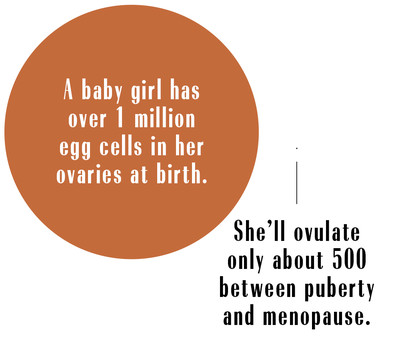
Not surprisingly, lots of people have lots of opinions about the prospect of women having children much later in life than is now typically possible. A primary concern, regardless of whether they use their own eggs or someone else’s: Will older moms be around to parent their children to adulthood?
In 2006, María del Carmen Bousada de Lara of Spain became the oldest documented woman to give birth, delivering twin boys conceived via IVF at 66. When she died of cancer before they turned three, critics were quick to say she had overstepped ethical boundaries, both by lying to the fertility clinic about her age and by deciding to get pregnant in the first place. In the U.S., “because of concerns related to the high-risk nature of pregnancy, as well as longevity,” the American Society for Reproductive Medicine (ASRM) has taken a stand, advising physicians against helping women older than 55 achieve pregnancy.
Whether it’s perceived as acceptable for a woman past conventional childbearing years to get pregnant hinges largely on what we as a society think about who is fit to be a mother, says Ruth Faden, founder of the Johns Hopkins Berman Institute of Bioethics. Ethically speaking, a child’s welfare is a key consideration, so Faden believes some sort of age limit is a good idea. “Children deserve vigorous, healthy parents who can get on the floor to play with them and who can see them through to young adulthood,” she says. “It’s one thing if parents have disabilities or illness that affects how they can parent, but if you’re talking about women wanting to become pregnant at, say, 70, it should start to raise concerns.”

Assistant professor Jennifer Garrison studies the brain’s role in female reproductive aging.
“People say older parents won’t survive for their child’s high school or college graduation, but so what?” asks Zaher Merhi, a fertility doctor at New Hope Fertility in New York City. “I might not survive. I might get killed in a car crash. Having babies is part of feeling young. If ASRM changed its guidelines, I’d support [helping women of] any age to get pregnant.”
On the other hand, age does play a role in how women tend to tolerate pregnancy. “If we look at this from a medical perspective, it seems pregnancy has been meant for the relatively young,” says Eli Adashi, an ob-gyn and former dean of Brown University’s medical school. “That’s not to say you can’t deal with it at 40, 50, or 60, but the longer you wait, the more medical issues you’re likely to acquire. Ethics requires that we respect personal decisions, but medicine would suggest we point out the advantages of early childbearing.”
For years, the scientific community studying aging didn’t consider reproductive aging part of its purview because women begin experiencing a decline in reproductive function in their 30s, not their 70s or 80s—the demographic more typically associated with gerontology. But the pendulum is starting to shift. Last year, the National Institute on Aging announced a special call for research proposals to shed light on the mechanisms that regulate how reproductive cells and tissues age. “This is a huge advance because both fields—reproductive science and aging—are acknowledging the critical value of this research area,” says Francesca Duncan, assistant professor in obstetrics and gynecology and executive director of the Center for Reproductive Science at Northwestern University. (She’s also an assistant professor in residence at the Buck Institute.) “Every female will experience ovarian aging, so this is an important model to study aging.”
Understanding what underpins reproductive aging is about much more than extending childbearing, says Duncan. Postponing ovarian aging will allow the ovaries to continue producing estrogen. After menopause, low levels of estrogen raise women’s risk of heart disease, stroke, and osteoporosis. “I want to help women live longer in a healthier state,” says Duncan.
Duncan’s research focuses on how oocytes—immature egg cells—and the environment in which they develop change with age. One of her fundamental discoveries is that cohesin (a protein that acts like a “molecular glue” holding chromosomes together until the right time and place) disintegrates with age. This glue is placed on chromosomes when oocytes are first formed during fetal development and has to remain functional until ovulation, which occurs decades later. Herein lies the problem: The ability of chromosomes to separate properly in the oocyte of a 45-year-old woman relies in part on the function of 45-year-old proteins. A breakdown in cohesin can cause chromosomal errors and lead to conditions such as Down syndrome.
It’s not as crazy as you might think to ponder putting off menopause or even doing away with it completely. Humans are fairly unique in going through it. Nearly all complex animals experience declining fertility as they age; only women and females of a few other species—beluga whales and narwhals and perhaps one type of monkey—lose their ability to reproduce in middle age.
There are plenty of theories about why women go through menopause. A primary one is that it served the greater good, says Judith Campisi, a pioneer in the field of cellular senescence (the study of how and why cells stop dividing) and a professor at the Buck Institute. Thousands of years ago, postmenopausal women were beneficial to hunter-gatherer and agricultural societies; older women who were no longer fertile could focus on helping with tasks unrelated to childbearing, plus they possessed valuable tribal memory. But no one is sure why women become infertile while men are able to father children into old age. “I’ve talked with evolutionary biologists,” says Campisi. “They say we don’t really know.”

Judith Campisi, a member of Shanahan's fertility squad, studies cell aging.
At her office at the Buck, Campisi’s colleague Lei ticks off some fun facts: The egg cell is the largest cell in the human body. At birth, a baby girl has one to two million eggs in her ovaries. She’ll end up ovulating only 500 or so times between starting puberty and then going through menopause. Lei is trying to understand what triggers a woman’s biological clock and the corresponding decline in egg quality and quantity. “That is key to extending fertility,” she says.
Most of her research is done on mice, which, like most mammals, have reproductive biology similar to that of humans. Peering through a microscope, Lei uses two tiny needles to liberate a mouse oocyte from its follicle for closer examination. Compared with a human ovary, a mouse ovary is a speck, no bigger than a kiwi seed.
Lei is standing in the lab with Shanahan, talking excitedly about the 300,000 oocytes present in a woman between puberty and adulthood. “Why do we use only about 500 of them?” she asks. “If we can use more, we can delay ovarian aging.”
Shanahan asks lots of questions, including why we as a society have taken for granted that women can’t have babies after middle age. Lei and the other scientists she meets with listen thoughtfully as they show Shanahan around the lab, pointing out incubators and microscopes, bought with her money, before assembling in a conference room with a view of the California live oak trees that dot the surrounding hills. It’s clear that Shanahan isn’t some benevolent but clueless benefactor. She understands that what these researchers are doing sounds like some futuristic fantasy. And she couldn’t be more thrilled that they’re thinking outside the box. “We’ve been looking through the lens of the patriarchy for so long”—accepting the status quo led by male researchers and doctors—“that perhaps it’s been making the obvious scientific steps less visible,” Shanahan says.
“I believe we are close to finding a noninvasive way to turn menopause on and off,” she says. “At the end of the day, women need to understand that the medical community should be and will [be] and is working on more opportunities for them to make choices for themselves. Some women may be ready for menopause, but for those who aren’t, there should be more options.”
As happens with some women struggling with infertility, Shanahan ended up conceiving naturally about eight months after she’d given up hope of getting pregnant. “We’re put here on this planet for a reason,” she says. Perhaps, despite the heartbreak that sparked her interest in reproductive equality, the long road she’d traveled had been worthwhile. “Maybe this was the insight that had to happen.”
Echo, Shanahan’s daughter with Brin, is now more than a year old. She likes noodles and tangerines and playing on the slides at the park. Shanahan hopes that by the time Echo might consider having a child of her own, she will have options for building a family that look very different from the ones her mother encountered.
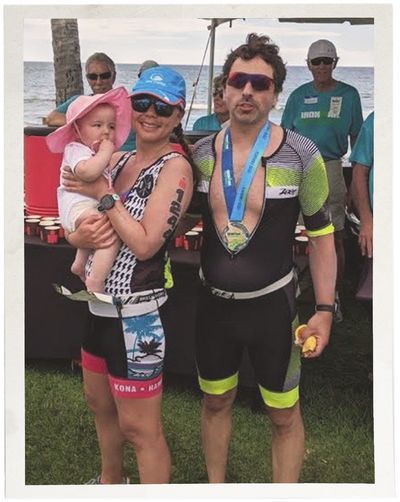
Shanahan and Brin with their daughter, Echo, celebrating the completion of a triathlon.
Editors’ note: We use the terms “woman” and “female” in this article to refer to people with internal reproductive organs; however, we understand that not everyone with internal reproductive organs identifies as a woman or a female. We use the terms “man” and “male” to refer to people with external reproductive organs; however, we understand that not everyone with external reproductive organs identifies as a man or a male.
For more stories like this, including celebrity news, beauty and fashion advice, savvy political commentary, and fascinating features, sign up for the Marie Claire newsletter.
subscribe here (opens in new tab)
RELATED STORIES
Bonnie Rochman has written for publications including The New York Times Magazine, The Wall Street Journal, The Washington Post and Scientific American. A former health and parenting columnist for Time magazine, she writes regularly about women’s health. Her book, The Gene Machine: How Genetic Technologies Are Changing the Way We Have Kids — and the Kids We Have, was named one of Amazon’s Top Science Books of 2017. Bonnie lives in Seattle with her husband and three children.
-
 The Queen Has Eaten This Food Every Day for the Past 91 Years
The Queen Has Eaten This Food Every Day for the Past 91 YearsNow that’s commitment!
By Rachel Burchfield
-
 Kate Middleton Altered Her Engagement Ring to “Avoid Her Worst Nightmare”
Kate Middleton Altered Her Engagement Ring to “Avoid Her Worst Nightmare”The ring was actually originally supposed to have been worn not by Prince William’s wife, but by Prince Harry’s (!).
By Rachel Burchfield
-
 Princess Diana Saw a Much Different Future for the Relationship Between Brothers Prince William and Prince Harry
Princess Diana Saw a Much Different Future for the Relationship Between Brothers Prince William and Prince HarryHow would she react to their feud if she were alive today?
By Rachel Burchfield
-
 I'm an Egg Donor. Why Was It So Difficult for Me to Tell People That?
I'm an Egg Donor. Why Was It So Difficult for Me to Tell People That?Much like abortion, surrogacy, and IVF, becoming an egg donor was a reproductive choice that felt unfit for society’s standards of womanhood.
By Lauryn Chamberlain
-
 Simone Biles Is Out of the Team Final at the Tokyo Olympics
Simone Biles Is Out of the Team Final at the Tokyo OlympicsShe withdrew from the event due to a medical issue, according to USA Gymnastics.
By Rachel Epstein
-
 Raven Saunders Is Getting Another Shot at Life—and the Gold
Raven Saunders Is Getting Another Shot at Life—and the GoldThe Olympic shot putter almost didn't live to see the Tokyo Games. Now, she's gearing up to compete while advocating for mental health in the sports world and beyond.
By Rachel Epstein
-
 After Years of Fertility Struggles I Had a Baby—and Then Twins 7 Weeks Later
After Years of Fertility Struggles I Had a Baby—and Then Twins 7 Weeks LaterM.M.LaFleur founder and CEO Sarah LaFleur shares her long, difficult, and surprising journey to parenthood.
By Sally Holmes
-
 Friendship, Infertility & Moving Forward
Friendship, Infertility & Moving ForwardThere’s no rulebook for navigating your pregnancy while your best friend struggles to conceive. I learned that the hard way.
By Victoria Lamson
-
 Changemakers 2021: Working Toward Wellness
Changemakers 2021: Working Toward WellnessPhysical and mental well-being cannot be separated. These changemakers are working to ensure you have both.
By Raquel Willis
-
 Don't Miss Frida's Realistic Breastfeeding Ad That Aired at the Golden Globes
Don't Miss Frida's Realistic Breastfeeding Ad That Aired at the Golden GlobesThe commercial accurately depicts the struggles of breastfeeding.
By Zoe Guy
-
 They Fled Domestic Violence in a Pandemic. Then Came the Winter Storm.
They Fled Domestic Violence in a Pandemic. Then Came the Winter Storm.Domestic abuse survivors in Dallas are facing trauma on top of trauma.
By Lorena O'Neil